Epilepsy and Seizures
Epilepsy is a multifaceted neurological disorder characterized by a heightened predisposition to recurrently generate epileptic seizures. Understanding the elevated risk of epilepsy among older adults holds significant importance for post-acute and long-term care providers, as it profoundly influences the assessment, care strategies, and overall well-being of their patients.
Etiology & Pathophysiology
Epileptic seizures in older adults can be caused by:
- Cerebrovascular Disease: Ischemic or hemorrhagic strokes can lead to scar formation in the brain, serving as a nidus for seizure activity.
- Neurodegenerative Disorders: Conditions like Alzheimer's disease can predispose to seizures.
- Brain Tumors: Primary or metastatic tumors may irritate surrounding brain tissue, provoking seizures.
- Infections: Encephalitis or meningitis can lead to seizures.
- Metabolic Derangements: Electrolyte imbalances, especially sodium and calcium, can affect neuronal activity.
- Traumatic Brain Injury: Even remote injuries can lead to post-traumatic epilepsy.
Clinical Assessment & Diagnosis
- History: An in-depth history helps to distinguish between an epileptic seizure and non-epileptic episodes. Witnesses' accounts of episodes are invaluable.
- Neurological Examination: Can sometimes reveal deficits post-seizure, known as Todd's paralysis.
- Electroencephalogram (EEG): Remains the gold standard for capturing seizure activity.
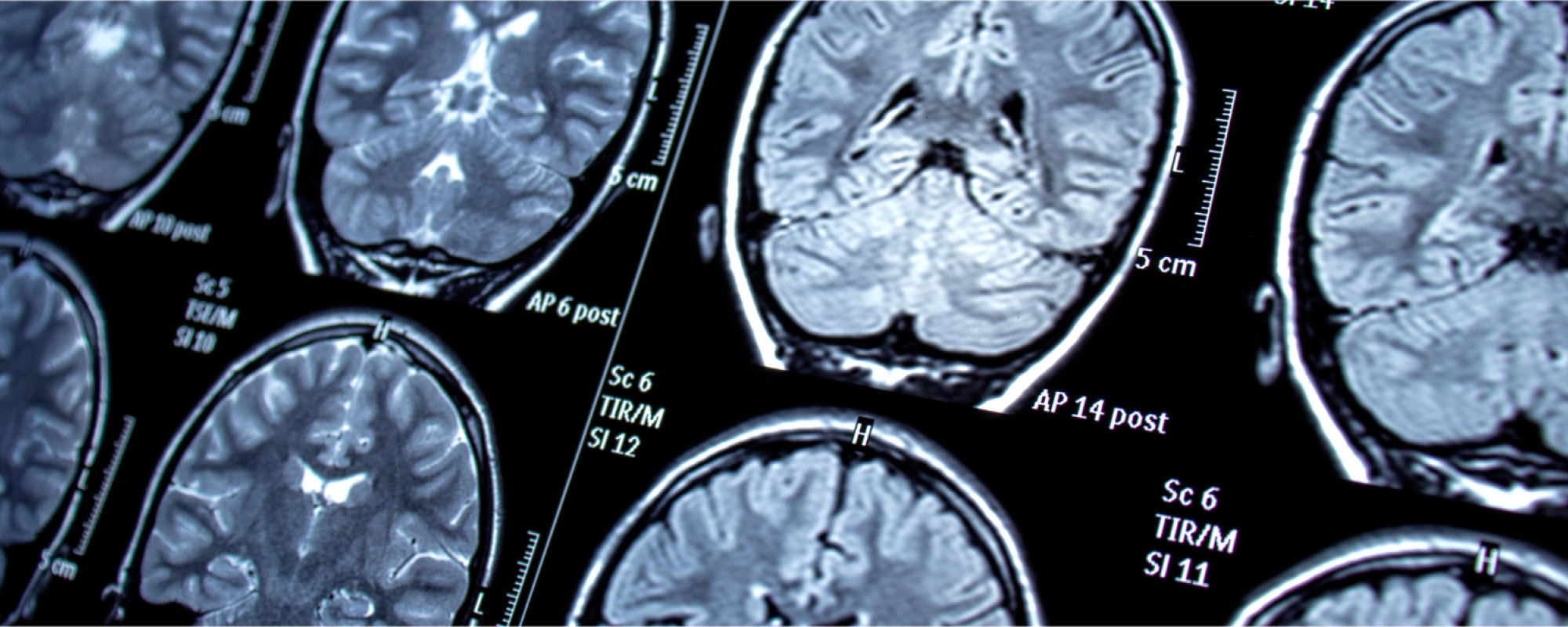
- Neuroimaging: MRI or CT scans can identify structural causes like tumors or strokes.
Management Strategies in PALTC
- Antiepileptic Drugs (AEDs): While several AEDs are available, prescribers should consider drug interactions, especially for older adults who are often on multiple medications. Common AEDs include levetiracetam, lamotrigine, and gabapentin.
- Lifestyle Advice: Ensuring good sleep hygiene, avoiding known seizure triggers, and moderating alcohol intake.
- Safety Precautions: Providing guidance on avoiding injury during a seizure, such as using safety helmets or avoiding certain activities.
- Regular Monitoring: Periodic EEGs and serum AED levels can optimize treatment.
Proactive Approaches & Care Considerations
- Interdisciplinary Collaboration: Neurologists, pharmacists, nursing staff, and caregivers must collaborate for optimal patient management.
- Education: Staff should be trained in seizure first aid, recognizing an impending seizure, and post-seizure care.
- Personalized Care Plans: Considering comorbidities, drug interactions, and the individual’s quality of life.