April 25, 2025
Measles activity is increasing in several areas of the United States, mainly among unvaccinated individuals. The Centers for Disease Control and Prevention provides weekly updates on measles cases on outbreaks on its website: https://www.cdc.gov/measles/data-research/index.html
About Measles
Measles is a highly contagious viral illness. The virus is transmitted by direct contact with infectious droplets or by airborne spread when an infected person breathes, coughs, or sneezes. Measles virus can remain infectious in the air and on surfaces for up to 2 hours after an infected person leaves an area.
Infected individuals are contagious from 4 days before rash onset through 4 days after.
- Incubation period to fever: ~7–10 days
- Incubation period to rash: ~10–14 days (range: 7–21 days)
Vaccination is the most effective way to prevent measles and control community outbreaks. Herd immunity is achieved when >95% of the population is immune.
Vaccine Effectiveness:
Virtually all children acquired measles in the US before the introduction of vaccines. People born before 1957 are assumed to have had the infection and considered immune. One dose of a measles vaccine (MMR) is 93% effective, and the recommended 2-dose series is 97% effective at preventing subsequent infection if exposed to measles. While this means that 3% of vaccinated people may still get measles if exposed to it, they will generally have a much milder illness and are less likely to spread the infection to others.
Implications for Long-Term and Post-Acute Care Facilities
In a non-outbreak regions
The focus of the Medical Director should be on prevention and readiness by:
- Verifying immunity of staff.
- Reviewing screening and isolation/work exclusion protocols and Personnel Protective Equipment (PPE) supplies.
- Educating staff about signs and symptoms of measles.
- Early signs and symptoms of measles include fever, cough, coryza and red, watery eyes (conjunctivitis)
- Measles rash appears 3 to 5 days after the first symptoms. It usually begins on the face and then spread downward to the neck, trunk, arms, legs, and feet.
- Discussing measles containment response plans with infection prevention and control team.
Resources:
- Interim Infection Prevention and Control Recommendations for Measles in Healthcare Settings | Infection Control | CDC
- Guidance on Measles Immunization (ACIP)
- Clinical Overview of Measles | Measles (Rubeola) | CDC
Assessing Immunity to Measles:
1. Healthcare Personnel:
Healthcare personnel (HCP) include anyone working in a healthcare setting who may be exposed to patients. Facilities should ensure that HCP have documentation of adequate vaccination against measles or are other acceptable evidence of immunity
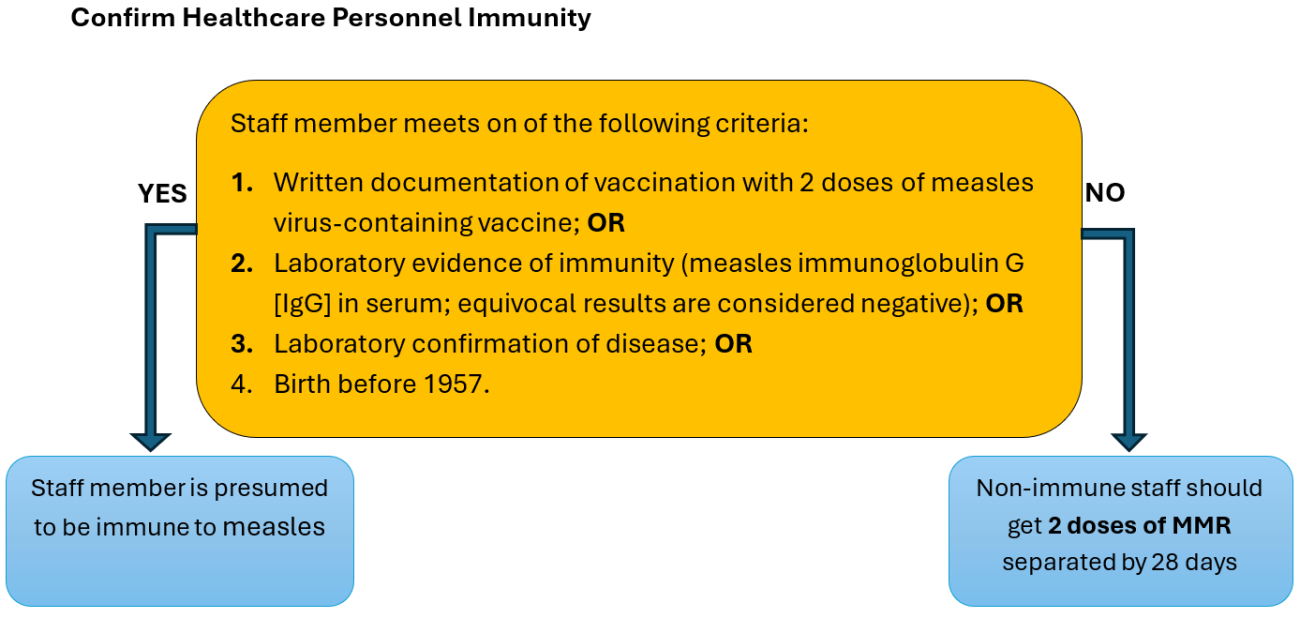
Note: Consider vaccinating HCP born before 1957 who lack laboratory evidence of immunity or laboratory confirmation of disease.
2. Residents:
In non-outbreak areas in the US, routine measles immunity screening or antibody testing is not recommended for adult residents.
Most adult residents in PALTC facilities are likely to be immune:
- Born before 1957: Presumed to have natural immunity due to widespread measles circulation prior to vaccination programs.
- Born in or after 1957 and before 1989: Likely received at least one dose of measles vaccine, which is still considered sufficient for protection in routine settings.
There is no recommendation for a catch-up program among adults for a second dose of MMR (e.g., persons born before 1989 or otherwise) in non-outbreak settings.
Resources:
- Guidance on Measles Immunization (ACIP)
- Questions About Measles | Measles (Rubeola) | CDC
- Routine MMR Vaccination Recommendations: For Providers | CDC
- Immunize.org Ask the Experts: MMR (Measles, Mumps, and Rubella)
- Measles-Playbook_March-2025.docx
In areas experiencing measles outbreaks
The Medical Director should:
- Monitor state and CDC health alerts and follow state and local public health guidance.
- Proactively review and document immunity of all staff.
- Educate staff and residents about signs and symptoms of measles.
- Implement enhanced entry screening for rash/fever.
- Inform healthcare personnel on infection control protocols for management of exposed healthcare personnel and those infected with measles.
- Be prepared to implement cohorting or quarantine strategies, if needed.
- Establish a communication plan for rapidly informing public health officials and families if a case is suspected.
1. For healthcare personnel:
- During a measles outbreak: 2 doses of measles virus-containing vaccine are recommended for all HCP, regardless of year of birth.
- If there is a suspected or confirmed measles case in the facility, work with public health to assess the need for post-exposure prophylaxis (PEP), symptoms monitoring and work exclusions.
- PEP is recommended for individuals without evidence of immunity against measles.
- PEP should be provided, as soon as possible after exposure, either with MMR vaccine (within 72 hours) or immunoglobulin (within 6 days). The choice of PEP is based on elapsed time from exposure or medical contraindications to vaccination (e.g. pregnancy or immunocompromised status).
- HCP without evidence of immunity against measles are recommended to be excluded from work from the 5th day after their first exposure through the 21st day after their last exposure, regardless of receipt of postexposure prophylaxis.
2. Residents:
- If there is a suspected or confirmed measles case in the facility, work with public health to assess need for post-exposure prophylaxis and immune status evaluation.
Resources:
- CDC Weekly Measles Surveillance Data
- Health Alert Network (HAN) - 00522 | Expanding Measles Outbreak in the United States and Guidance for the Upcoming Travel Season
- CDC Interim Infection Control Guidance for Measles in Healthcare Settings
- Measles Update — United States, January 1–April 10, 2025
- Measles | Infection Control | CDC
Appendix A: Measles Preparation and Response Checklist for PALTC Facilities
Non-Outbreak Settings
☐ | Verify immunity of staff |
☐ | Review screening and isolation/work exclusion protocols using CDC guidance as a reference |
☐ | Review personal protective equipment (PPE) supplies |
☐ | Educate staff about early signs and symptoms of measles using CDC guidance as a reference |
☐ | Discuss measles containment response plans with infection prevention and control team using CDC guidance as a reference |
Outbreak Settings
☐ | Follow any state and local public health guidance |
☐ | Monitor state and CDC health alerts
|
☐ | Proactively review and document immunity of all staff
|
☐ | Educate staff and residents about signs and symptoms of measles using CDC guidance as a reference |
☐ | Inform healthcare personnel on infection control protocols for management of exposed healthcare personnel and those infected with measles |
☐ | Prepare to implement cohorting or quarantine strategies, if needed |
☐ | Establish a communication plan for rapidly informing public health officials and families if a case is suspected |
☐ | If suspected or confirmed measles case in the facility: work with public health to assess needs for immune status evaluation of residents, post-exposure prophylaxis for staff and residents, symptoms monitoring for exposed staff and work exclusions |